 |
|
Bios Drs. Levinger and Cruz Pimentel are vitreoretinal fellows at the University of Toronto. |
The positioning of the head following gas injection during pneumatic retinopexy and the interaction of the gas bubble with the retina are critical in successful management and resolution of rhegmatogenous retinal detachment.1 The intraocular gas must be in the appropriate position, and the relationship between gas bubbles and residual vitreous fluid shows a significant change when a patient’s head position changes. Poor positioning may lead to inadequate contact, increasing the risk of failure.
This article will briefly review some of the current concepts, and evolving strategies for head positioning following PnR in the management of RRD.
The gas injection technique
When selecting a gas for pneumatic retinopexy, two key considerations are the required duration of tamponade and the desired bubble size. Sulfur hexafluoride (SF6), the most commonly used gas,2,3 expands rapidly within 24 to 36 hours and is absorbed in seven to 10 days, making it ideal for rapid, effective tamponade. Perfluoropropane (C3F8), which expands more slowly and lasts longer, is reserved for cases requiring prolonged support. In our practice, filtered SF6 is drawn from a large tank into a syringe after anterior chamber paracentesis. Gas is injected 3.5 to 4 mm from the limbus into a flat area of the superior retina, aiming for a large bubble (0.3 cc for C3F8 and 0.6 cc for SF6). Patients are then leaned forward to allow fluid redistribution, followed by a second anterior chamber paracentesis. While initial “fish egg” bubbles often coalesce within 48 hours, injecting less deeply into the vitreous cavity reduces complications and partial needle withdrawal can help avoid bubble fragmentation.
Steamroller maneuver
Paul Tornambe, MD, and George Hilton, MD, introduced the steamroller maneuver for flattening retinal detachments using an injected intravitreal gas bubble to direct subretinal fluid from the subretinal space through the retinal break into the vitreous cavity. This technique has three primary objectives: (1) expedited apposition of the macula in cases characterized by a fovea-off detachment; (2) minimization of fluid movement toward the macula in instances of fovea-on detachment; and (3) facilitation of SRF drainage toward the vitreous cavity in cases with superior bullous RRD.4,5
The direct-to-the-break technique has been proposed to decrease the potential hypothetical risk of PVR from the steamroller maneuver,6 and provide more comfort to the patients following PnR. This technique involves positioning the patient’s head in the direction where the gas bubble closes the break immediately after injection. However, this approach comes with notable disadvantages. While it may provide greater comfort for patients, especially older ones, direct positioning toward the break can delay retinal attachment. Additionally, the gas bubble’s immediate closure of the causative break can inadvertently push subretinal fluid toward areas with unseen breaks or previously treated breaks in the attached retina, resulting in a higher rate of treatment failures. It’s essential to weigh these risks carefully when considering this positioning strategy.
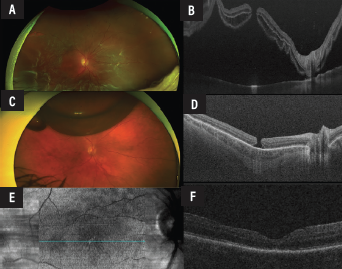 |
| Figure 1. Representative case of a 62-year-old patient with a rhegmatogenous retinal detachment with several breaks in the temporal quadrant and a full-thickness macular hole in the right eye (A-B). The preoperative gas for pars plana vitrectomy or “PGP technique” was used, followed by laser retinopexy at 48 hours (C-D). The patient also underwent pars plana vitrectomy with inverted internal limiting membrane flap technique within one week. Postoperatively, this complex case had a good anatomical outcome (E-F). |
A study conducted to explore the impact of head positioning in patients treated with PnR found no difference in terms of PVR rate between direct to the break and steamroller techniques when argon laser is used to create retinopexy.7 The single-operation success rates were 74 percent for the basic technique and 67 percent for the steamroller technique, with overall success reaching 100 percent in both groups after reoperations. Postoperative visual acuity improved significantly in both groups, with no statistically significant difference in final outcomes, although the steamroller group trended toward better visual acuity.
Alternatives such as the Mini Steamroll technique,8 which involves brief face-down positioning (approximately 10 minutes) followed by direct-to-break positioning in cases of significant bullous detachments have also been proposed. These findings suggest that both techniques are equally viable for PnR in cases with superior, small retinal breaks, though further large-scale studies are needed for definitive conclusions.
Importance of precise positioning
A recent study used high-resolution orbital MRI imaging to demonstrate the dependency of contact between the gas bubble and retina on accurate head positioning.9 The study findings demonstrated that among the positioning options—prone, supine, right side and left side—both side and prone positions have the potential for supporting peripheral anterior retinal breaks. Side positioning, however, produces better contact for anterior inferior retina than prone positioning. Small deviations from ideal prone posture reduced inferior retinal contact, emphasizing how critical precise positioning is postoperatively. As such, side positioning may offer a more effective and practical alternative to face-down positioning for supporting inferior retinal breaks. Additionally, incomplete gas fill or inaccurate positioning resulted in inadequate retina support.9 A separate study found that maintaining an acceptable head position after PnR is challenging, with proper positioning achieved for only 3.33±1.8 hours.10
Pearls for PnR • Steamrolling can initially help the macular SRF • Consider side positioning for PnR • SF6 gas is our first choice •Steamroll: Initial four hours face down • PGP is highly effective and easy to incorporate into your practice |
Preoperative gas for pars plana vitrectomy (PGP)
The PGP technique offers the benefits of a higher anatomic success rate as well as the accessibility and functional benefits of PnR.11 In a case series of all RRDs between January 2016 and January 2020 who underwent PGP at our institution (Toronto Western Hospital, University of Toronto) the PGP technique as an adjunct to the surgical repair of RRD was found to have an anatomical success rate of 95 percent.11 In addition, PGP was noted to enhance the ease of surgery and improve functional as well as anatomical success. For patients with inferior breaks, using a large gas bubble and face-down positioning may promote foveal reattachment while awaiting vitrectomy.
For macula-on RRDs, good patient positioning with PGP can prevent extension into the macular region of retinal detachment before PPV, thus protecting the macula. The use of PGP as an adjunct to PPV also reduces surgical costs, enhances ease of the surgery and need for retinotomy. In cases with superior breaks larger than one clock hour that don’t meet the traditional criteria for PnR, PGP can lead to significant reattachment of the superior retina and reduce the need for use of perfluorocarbon liquid drainage of subretinal fluid.
Putting it all together
Optimizing head positioning following PnR is essential to achieving successful anatomical and functional outcomes in the repair of RRD. While traditional prone positioning remains widely used, evolving evidence—including high-res MRI studies—suggests that side positioning may provide superior tamponade of the anterior inferior retina, especially when gas fill is incomplete or precise alignment is challenging.
Techniques such as the steamroller maneuver, direct-to-break positioning, and mini-steamroll each offer unique advantages and limitations, reinforcing the need for individualized posturing strategies based on break location, gas fill and patient-specific factors. In our practice, we routinely use SF6 gas to ensure a large initial bubble to reattach the macula. A steamroll of approximately four hours face down followed by side positioning ensures a rapid macular reattachment followed by a more comfortable and reliable side position for the patient.
The addition of preoperative gas for pars plana vitrectomy to our practice offers promising anatomical and surgical benefits in RRD and is routinely done for patients in which standard PnR is likely to be unsuccessful (inferior tears, unlikely to comply with positioning, hazy media not amenable to post-gas laser retinopexy). In vitreoretinal practices that currently don’t use PnR, PGP offers an excellent starting point from which to implement the functional benefits of PnR into your practice, while still enjoying the anatomical success of PPV. Future research should continue to refine positioning protocols to maximize reattachment success while minimizing patient burden and complication risk for RRD repair. RS
References
1. Mandelcorn ED, Mandelcorn MS, Manusow JS. Update on pneumatic retinopexy. Curr Opin Ophthalmol. 2015;26:194–199.
2. Stewart S, Chan W. Pneumatic retinopexy: patient selection and specific factors. Clin Ophthalmol. 2018 Mar 16;12:493-502.
3. Ai E, Gardner TW. Current patterns of intraocular gas use in North America. Arch Ophthalmol. 1993 Mar;111:3:331-2.
4. Hilton GF, Kelly NE, Salzano TC, Tornambe PE, Wells JW, Wendel RT. Pneumatic retinopexy. A collaborative report of the first 100 cases. Ophthalmology. 1987;94:4:307-314.
5. Tornambe PE, Hilton GF. Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. The Retinal Detachment Study Group. Ophthalmology. 1989;96:6:772-784.
6. Tornambe PE, Hilton GF. The steamroller maneuver and proliferative vitreoretinopathy. Arch Ophthalmol. 1992;110:1:15.
7. Yanyali A, Horozoglu F, Bayrak YI, Celik E, Nohutcu AF. Steamroller versus basic technique in pneumatic retinopexy for primary rhegmatogenous retinal detachment. Retina. 2007;27:1:74-82.
8. Pecaku A, El-Sehemy A, Melo IM, et al. THE MINI-STEAMROLL: An abbreviated variation of the steamroller maneuver after pneumatic retinopexy for rhegmatogenous retinal detachment. Retina. 2024;44:11:1876-1883.
9. Hostovsky A, Mandelcorn M, Mandelcorn E. Orbital magnetic resonance imaging demonstrates better contact between the gas and anterior inferior retina in side versus face-down position. Ophthalmol Retina. 2020;4:9:911-918.
10. Velez-Montoya R, León AG, Hernández-Quintela E. Assessment of postural compliance after pneumatic retinopexy. Transl Vis Sci Technol. 2019;8:3:4.
11. Felfeli T, Mandelcorn MS, Trussart R, Mandelcorn ED. Preoperative gas for pars plana vitrectomy: A surgical technique for repair of rhegmatogenous retinal detachments with multiple, large, or inferior breaks. Retin Cases Brief Rep. 2023;17:4:374-379.




