 |
Bios Dr. Felfeli is an ophthalmology resident at the Univeristy of Toronto. Dr. Córdoba-Ortega is a Dr. Arias Aristizábal is a retina and ocular oncology specialist at the Foscal Internacional – FOSUNAB. DISCLOSURES: The authors have no relevant disclosures. |
Sturge-Weber syndrome is associated with ocular complications, including glaucoma and diffuse choroidal hemangiomas, which can lead to severe exudative retinal detachments that are challenging to treat and require a specialized multidisciplinary approach.1
Common therapeutic options, such as photodynamic therapy and transpupillary thermotherapy, may be limited, and vitrectomy, although necessary in severe cases, can present significant challenges, especially in cases of total retinal detachment with a closed funnel configuration.2,3
External subretinal fluid drainage is an effective option for treating exudative retinal detachments,4 particularly in cases associated with diffuse choroidal hemangioma in Sturge-Weber syndrome when conventional methods aren’t effective.
Our case
Our 19-year-old male patient with Sturge-Weber syndrome had a total exudative retinal detachment with a closed-funnel configuration, caused by diffuse choroidal hemangioma. The complexity of the detachment hindered direct visualization of the tumor, limiting therapeutic options.
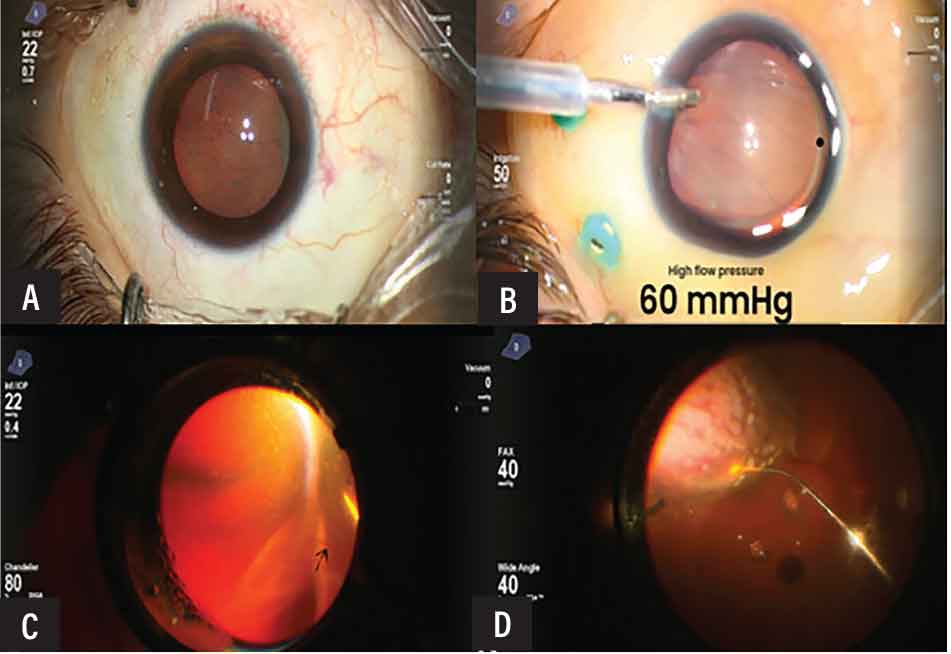
Intraoperatively, we observed that the retina was adherent to the posterior capsule of the lens (Figure A), so we decided to perform external drainage of the subretinal fluid (Figure C) because otherwise it was difficult to visualize and directly treat the hemangioma. An anterior chamber maintainer allowed precise control over retina expansion and subretinal fluid manipulation (Figure B).
We then completed a posterior vitrectomy with perfluorocarbon and air, which stabilized the retina, improved peripheral visualization, and prevented interface bleeding, along with preserving the lens in a young patient.
We then applied laser pulses to the tumor, and completed the procedure with a 20% SF6 gas exchange (Figure D). We chose laser as a viable alternative to photodynamic therapy,5-7 which was unavailable.
 |
|
A) Retina adherent to the posterior capsule of the lens due to total retinal detachment with a closed funnel configuration. B) The anterior chamber maintainer in use. Note the displacement of the retina toward the posterior plane. C) External drainage with a needle guided under direct visualization. D) Air interface vitrectomy and laser treatment over the entire tumor. |
Applying laser in the context of total retinal detachment with a closed funnel configuration presents significant challenges, particularly because parallax effects cause limited visualization of the tumor. This issue complicates the proper application of treatment and subsequent follow-up, especially given that the patient is young and phakic.
In such cases, it’s preferable to avoid retinotomies, because they could increase the risk of redetachment and the formation of proliferative vitreoretinopathy. In young patients, lens preservation becomes a priority, necessitating a carefully designed surgical approach.
Here, interface vitrectomy is crucial. Operating under air enhances peripheral visualization, prevents bleeding and controls subretinal fluid, facilitating the adaptation of the retina toward the posterior pole. Incorporating external drainage and the use of a high-pressure anterior chamber maintainer allow for adequate stabilization before addressing the hemangioma and ensuring precise follow-up. This comprehensive strategy not only optimizes surgical outcomes, but also significantly contributes to preserving visual function and enhancing the patient’s long-term quality of life.
Postoperative follow-up demonstrated successful reattachment of the retina, with significant reduction of subretinal fluid and improved visual acuity, reaching 20/100 at six months. We used oral propranolol as an adjunctive therapy, with no recurrences or additional complications.
Bottom line
Exudative retinal detachment is a severe complication of diffuse choroidal hemangioma and poses significant challenges because of the complexity and aggressiveness of the condition. External subretinal fluid drainage can be an effective option for cases that don’t respond to conventional methods. Our approach not only enabled effective retinal reattachment, but also facilitated targeted tumor treatment and patient rehabilitation. RS
REFERENCES
1. Sabeti S, Ball KL, Bhattacharya SK, et al. Consensus statement for the management and treatment of Sturge-Weber syndrome: Neurology, neuroimaging, and ophthalmology recommendations. Pediatr Neurol. 2021;121:59-66.
2. Sánchez-Espino LF, Ivars M, Antoñanzas J, Baselga E. Sturge-Weber syndrome: A review of pathophysiology, genetics, clinical features, and current management approache. Appl Clin Genet. 2023;16:63-81. Erratum in: Appl Clin Genet. 2024;17:131-132.
3. Thapa R, Shields CL. Oral propranolol therapy for management of exudative retinal detachment from diffuse choroidal hemangioma in Sturge-Weber syndrome. Eur J Ophthalmol. 2013;23:922-924.
4. Felfeli T, Grewal PS, Mandelcorn ED. Applications of the guarded-needle external drainage technique in vitreoretinal surgery. Retina. 2023;43:2130-2133.
5. Jurklies B, Bornfeld N. The role of photodynamic therapy in the treatment of symptomatic choroidal hemangioma. Graefes Arch Clin Exp Ophthalmol. 2005;243:393-336.
6. Huiskamp EA, Müskens RP, Ballast A, Hooymans JM. Diffuse choroidal haemangioma in Sturge-Weber syndrome treated with photodynamic therapy under general anaesthesia. Graefes Arch Clin Exp Ophthalmol. 2005;243:727-730.
7. Anand R. Photodynamic therapy for diffuse choroidal hemangioma associated with Sturge Weber syndrome. Am J Ophthalmol . 2003;136:758-760.




