 |
Bios Dr. Tan is a vitreoretinal surgery fellow, and currently undertaking a PhD at the University of Oxford. |
Full-thickness macular holes (FTMHs) can sometimes occur in conjunction with rhegmatogenous retinal detachments. The reported incidence of this occurrence is low (1.6 to 2.3 percent of all RRDs), but may be more common in the presence of proliferative vitreoretinopathy.1 Closure of the FTMH is not a pre-requisite for successful retinal re-attachment. Nevertheless, a variety of surgical techniques aimed at FTMH closure in this setting have been described, such as internal limiting membrane peel, with or without an ILM flap.2-3 In the presence of very large FTMHs, other adjunctive measures may be required, such as the use of autologous blood, amniotic membrane grafts or retinal autografts, each of these with their own advantages and disadvantages.4-6
Here we provide our experience and tips for a challenging case with a large secondary macular hole in a highly myopic PVR re-detachment. We used a retinal autograft with retinectomy and the Sub-Perfluorocarbon Ophthalmic viscoelastic device Tamponade (SPOT) technique, in this case with a good outcome.7
The case
This was an eye with high myopia, that presented with retinal re-detachment and PVR, after a previous combined scleral buckle, vitrectomy, ILM peel and gas tamponade. Intraoperatively, we found a large secondary FTMH. Given that we already intended to perform an inferior retinectomy, we took the opportunity to harvest a free retinal autograft from within the area of planned retinectomy. We suggest that in cases where a peripheral retinectomy is already going to be performed, harvesting a retinal autograft at the same time comes with little to no downside.
To prevent loss of the retinal autograft, we leave a pedicle when harvesting—this helps to keep the autograft in place until it’s ready to be moved to the macula. We also position the retinal autograft under perfluorocarbon liquid (PFCL). Using the SPOT technique, the retinal autograft is further stabilized with dispersive ophthalmic viscoelastic device injected over the graft-PFCL interface using a soft-tip cannula.7 During fluid-air exchange, the PFCL is carefully removed, leaving OVD over the retinal autograft for stabilization.
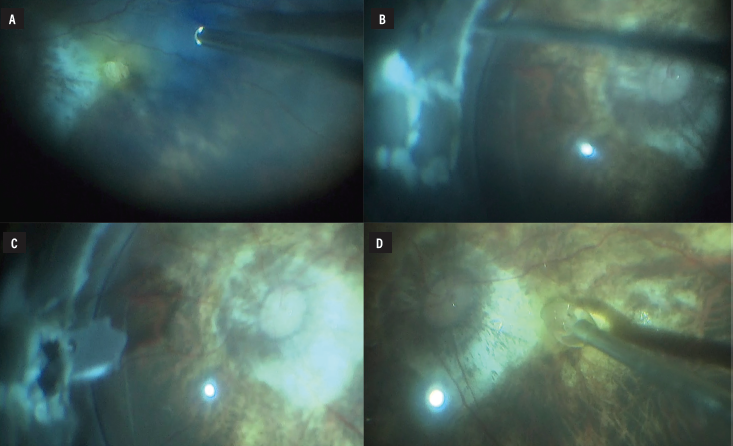 |
| Figure 1. Large secondary macular hole on a background of myopic maculopathy (A). Area of retinal autograft harvest marked out with endodiathermy, within the area of planned retinectomy (B). Retinal autograft cut and harvested, leaving a small pedicle (C). Ophthalmic viscoelastic device being injected with a soft tip cannula over the retinal autograft (D). |
The rationale for using OVD is to stabilize adjunctive flap and graft materials over macular holes, and reduce the risk of postoperative dislocation.7,8 Injection of OVD under PFCL is preferred as the high interfacial tension between OVD and PFCL makes the OVD less likely to disperse before coming into contact with the flap or graft.
Favorable results have been reported using the SPOT technique together with different flap and graft materials for refractory macular holes.8,9
The bottom line
A retinal autograft can be a good adjunct technique for large FTMHs, especially in cases where a peripheral retinectomy is already planned. Using OVD with the SPOT technique can be a useful way to stabilize retinal autografts or other flap materials over a FTMH. RS
REFERENCES
1. Cunningham MA, Tarantola RM, Folk JC, et al. Proliferative vitreoretinopathy may be a risk factor in combined macular hole retinal detachment cases. Retina. 2013;33:579–585.
2. Ryan EH, Bramante CT, Mittra RA, et al. Management of rhegmatogenous retinal detachment with coexistent macular hole in the era of internal limiting membrane peeling. Am J Ophthalmol. 2011;152:815-819.e1.
3. Stappler T, Montesel A, Konstantinidis L, et al. Inverted internal limiting membrane flap technique for macular hole coexistent with rhegmatogenous retinal detachment. Retina. 2022;42:1491–1497.
4. Khaqan HA, Sahyoun J-Y, Haider MA, Buksh HM. Amniotic membrane graft for the treatment of large refractory macular hole. Retina. 2022;42:1479–1483.
5. Lyu W-J, Ji L-B, Xiao Y, et al. Treatment of refractory giant macular hole by vitrectomy with internal limiting membrane transplantation and autologous blood. Int J Ophthalmol. 2018;11:818–822.
6. Grewal DS, Charles S, Parolini B, et al. Autologous retinal transplant for refractory macular holes: Multicenter International Collaborative Study Group. Ophthalmology. 2019;126:1399–1408.
7. Lai C-C, Wu A-L, Chou H-D, et al. Sub-perfluoro-n-octane injection of ocular viscoelastic device assisted inverted internal limiting membrane flap for macular hole retinal detachment surgery: A novel technique. BMC Ophthalmol 2020;20:116.
8. Chou H-D, Chong Y-J, Teh WM, et al. Nasal or temporal internal limiting membrane flap assisted by sub-perfluorocarbon viscoelastic injection for macular hole repair. Am J Ophthalmol. 2021;223:296–305.
9. Chen Y-T, Lai C-C, Hwang Y-S, et al. A surgical approach for managing refractory macular holes using the human amniotic membrane patch technique. Ophthalmic Surg Lasers Imaging Retina. 2024;55:613–616.




