 |
|
Bio Dr. Bowe is a vitreoretinal surgery fellow at Wills Eye Hospital/Mid-Atlantic Retina. |
A 6-month-old girl presented with esotropia since birth and concern for a retinal detachment. She was born full term and didn’t have any past medical history.
Workup and Imaging
In the office, a left esotropia was noted. The right and left eyes were white and quiet with unremarkable anterior segments and clear lenses. Limited fundoscopic examination of the right eye demonstrated clear vitreous, normal optic disc and flat periphery and posterior pole with unremarkable vasculature. Fundoscopic examination of the left eye also demonstrated clear vitreous with a large, peripapillary posterior staphyloma and optic disc anomaly. There was peripheral scarring noted without evidence of a rhegmatogenous retinal detachment.At this time, the differential diagnosis included morning glory syndrome, optic nerve coloboma and peripapillary staphyloma. The patient was taken for an examination under anesthesia.
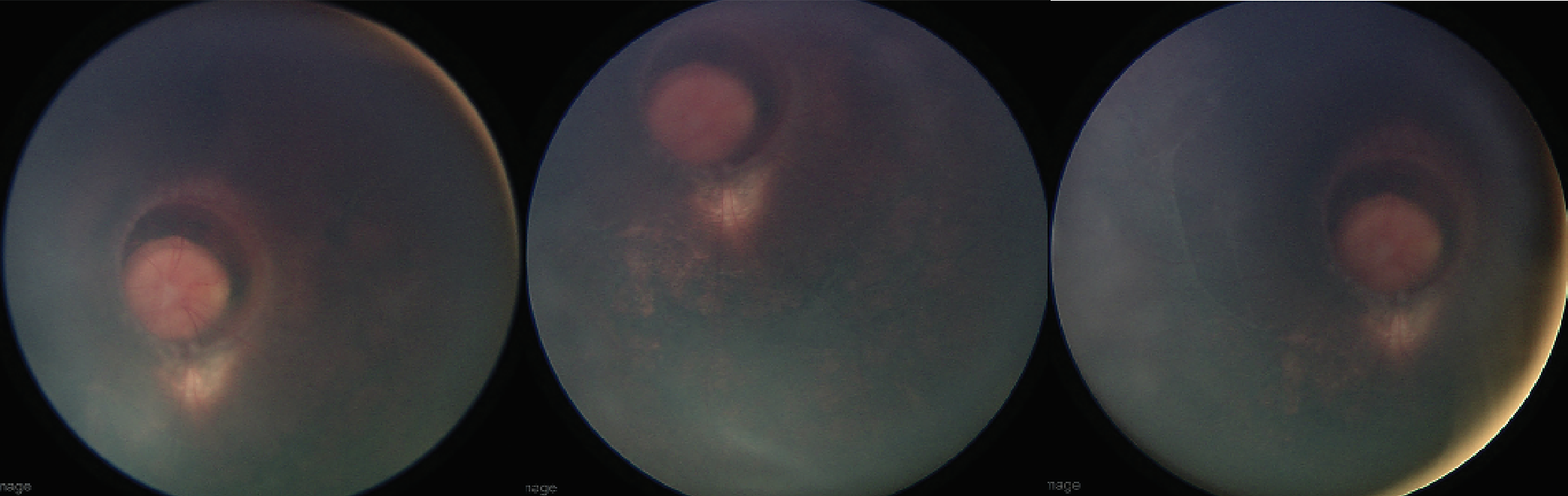
During the examination under anesthesia, the right fundus was confirmed to be normal. The left fundus was noted to have a deep set, enlarged optic disc with a glial tuft and peripapillary pigmentary changes consistent with morning glory disc anomaly (Figure 1). This morning glory disc was set back into a large peripapillary cyst.
 |
|
Figure 1. Color fundus photography revealed a deep set, enlarged optic nerve disc with a glial tuft within a large peripapillary staphyloma with cyst. |
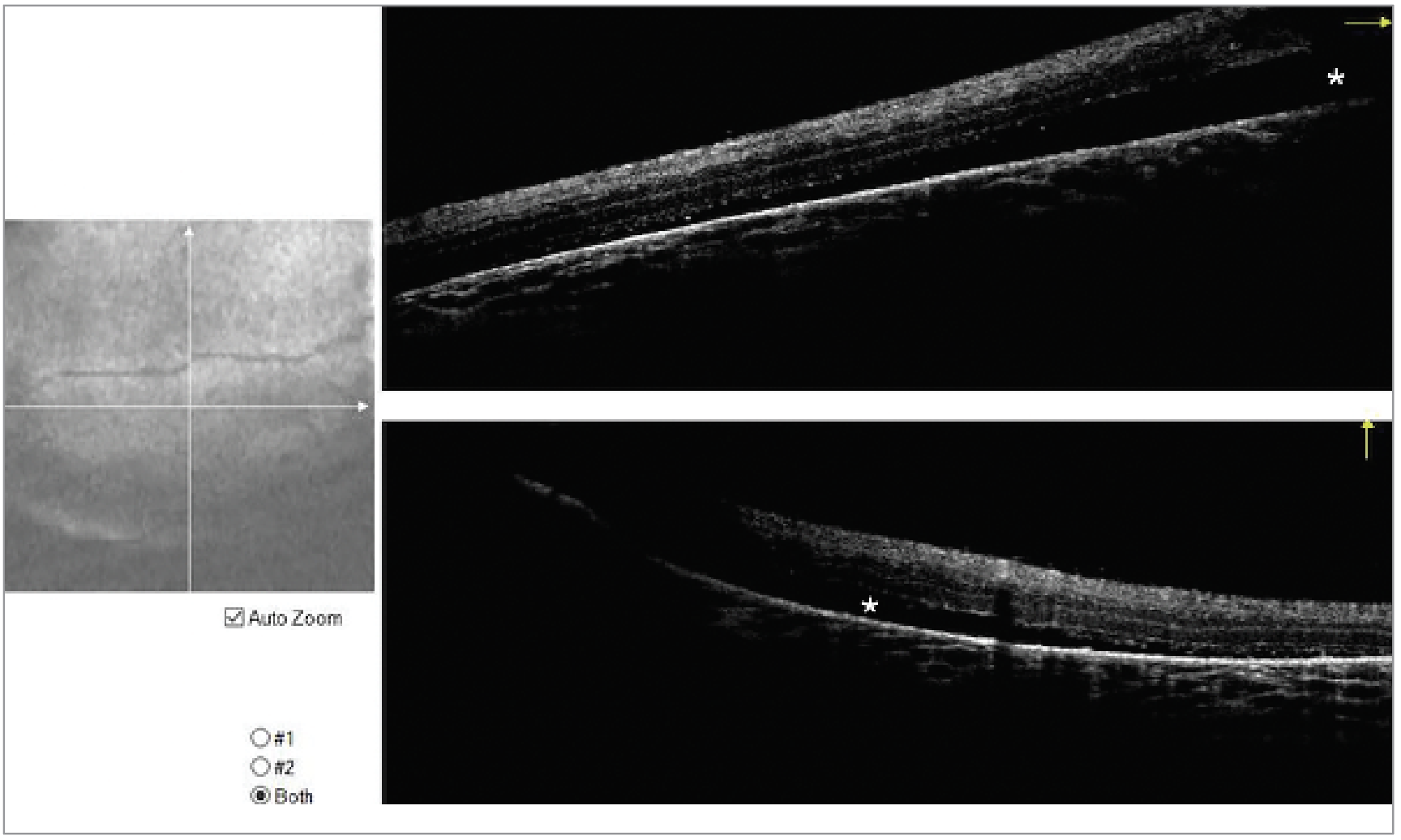
There was subretinal fibrosis and shallow, low lying temporal subretinal fluid. OCT confirmed shallow temporal subretinal fluid (Figure 2).
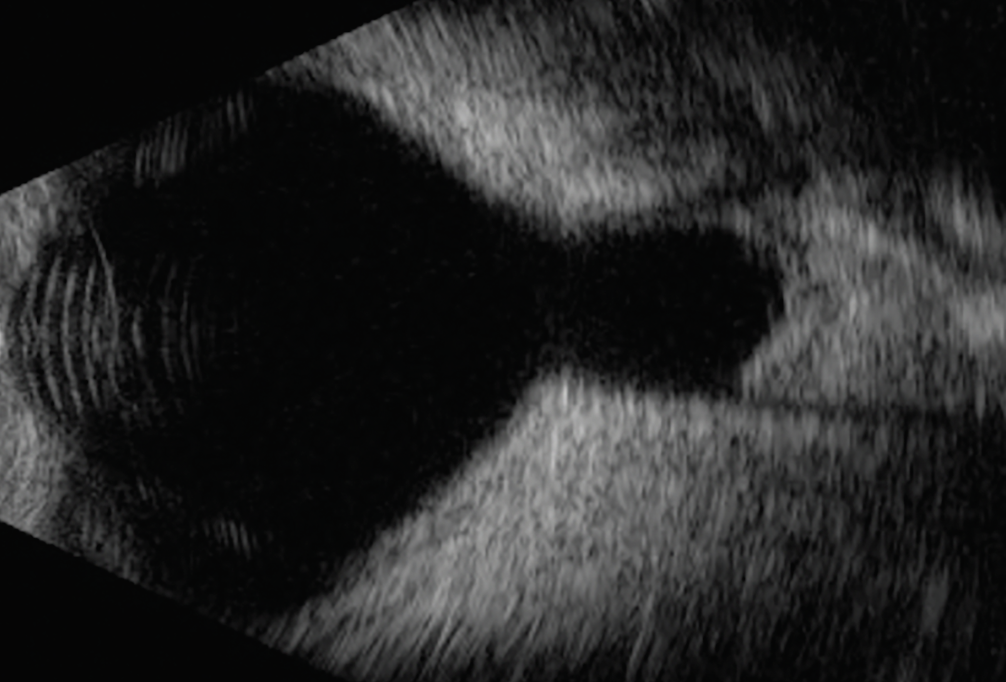
Intraoperative B scan ultrasonography revealed a large peripapillary staphyloma with cyst (Figure 3).
We diagnosed the patient with morning glory disc anomaly and arranged for outpatient neuroimaging.
 |
|
Figure 2 . Intraoperative OCT of the left eye demonstrating shallow subretinal fluid in the temporal macula. |
Discussion
Morning glory syndrome is a sporadic congenital optic disc anomaly characterized by an enlarged, funnel-shaped optic nerve head with surrounding conical excavation filled with central glial tissue, peripapillary chorioretinal pigmentary abnormalities and straightened retinal vessels.1
MGS is typically diagnosed prior to the age of 2.1 There’s no gender predilection. Presenting symptoms include strabismus, which can be present in as many as 80 percent of cases, along with abnormal visual behavior.1 There’s typically significant refractive error and the visual prognosis of the affected eye is poor.1 The pathophysiology isn’t clearly understood, and it may exist on a spectrum with other congenital optic disc anomalies including optic disc pit, coloboma and megalopapilla. Proposed mechanisms include a primary mesenchymal abnormality, which is consistent with the contractile nature of the glial tissue.2 The gliosis and vascular abnormalities suggest possible neuroectodermal dysgenesis.2
 |
|
Figure 3. B scan ultrasonography of the left eye demonstrating a large peripapillary staphyloma with cyst. |
Morning glory syndrome can be confused with cavitary optic disc anomaly, which can be inherited autosomal dominantly and is typically bilateral, whereas MGS is typically unilateral and sporadic.1 Other conditions that can mimic MGS include optic disc pit, which is a unilateral gray excavation of a portion of the optic disc. This can lead to visual impairment from subretinal fluid, intraretinal fluid, peripapillary staphyloma, glaucomatous optic neuropathy or optic nerve head coloboma.
In morning glory syndrome, visual impairment is often caused by anisometropic and strabismic amblyopia, along with associated retinal pathology. Peripheral non-perfusion can be present and can be found on fluorescein angiography. Retinal detachment can be present.
One report found that retinal detachment is found in 38 percent of cases.4 Detachments most often involve the posterior pole, however, they can progress to involve the peripheral retina.4 Additionally, there can be associated intraretinal fluid. The proposed mechanism of retinal detachment in MGD is vitreous traction at the nerve and macula leading to small microbreaks. Detachments are typically tractional in nature.4
One study supported the theory that the subretinal fluid is from a communication between cerebrospinal fluid and subretinal fluid (hypothesized to be pumped into the subretinal space via contractile motion of the glial tissue) by injecting a contrast dye intrathecally which was then found in the subretinal space on imaging.5 Visual acuity is generally 20/200 or worse, even in patients without retinal detachments or intraretinal fluid.6
MGS can be associated with systemic diseases, most commonly involving the face and central nervous system.6 Most critically, basal encephaloceles and moyamoya disease may be associated with MGS. Neuroimaging including CT and MRI should be performed to screen for these conditions. Moyamoya means “puff of smoke” in Japanese and was described in the literature in 1969.7 The disease is named for the characteristic diffuse and tangled angiographic appearance of the collateral vessels in the brain that form secondary to narrowing of the internal carotid artery and its major intracranial branches.7 It can result in significant neurologic morbidity due to complications such as stroke and seizure. 7
Bottom Line
MGS is a sporadic mesenchymal optic disc abnormality that presents in infancy or early childhood, has a poor visual prognosis regardless of intervention and requires additional neuroimaging to rule out serious neurologic and vascular conditions. RS
1. Cennamo G, de Crecchio G, Iaccarino G, Forte R, Cennamo G. Evaluation of morning glory syndrome with spectral optical coherence tomography and echography. Ophthalmology. 2010;117:6:1269-73.
2. Jain N, Johnson MW. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol. 2014;158:3:423-35.
3. Chang S, Gregory-Roberts E, Chen R. Retinal detachment associated with optic disc colobomas and morning glory syndrome. Eye (Lond). 2012;26:4:494-500.
4. Inoue M. Retinal complications associated with congenital optic disc anomalies determined by swept source optical coherence tomography. Taiwan J Ophthalmol. 2016;6:1:8-14.
5. Coll GE, Chang S, Flynn TE, Brown GC. Communication between the subretinal space and the vitreous cavity in the morning glory syndrome. Graefes Arch Clin Exp Ophthalmol. 1995;233:7:441-3.
6. Lit ES, D’Amico DJ. Retinal manifestations of morning glory disc syndrome. Int Ophthalmol Clin. 2001;41:1:131-8.
7. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:3:288-99.